Health watch

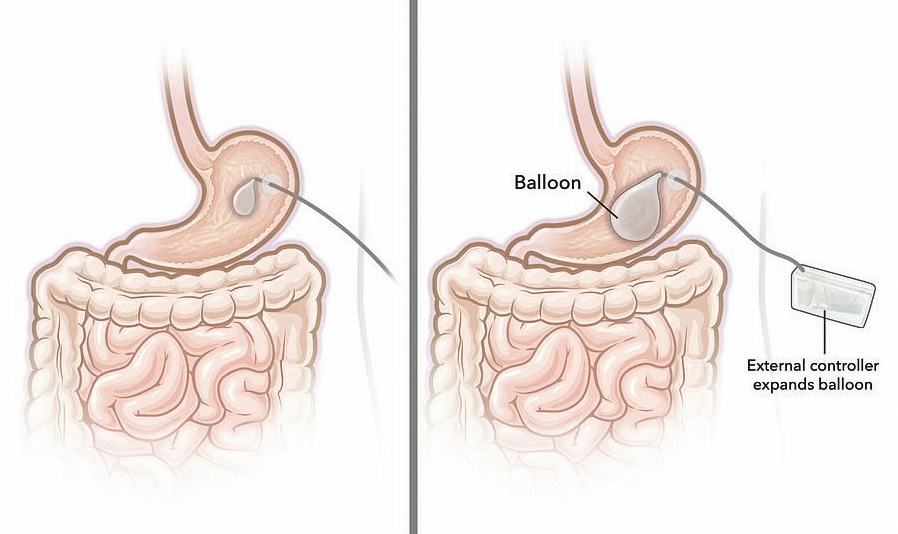
Users would be able to inflate the stomach balloon before a meal

alternative to traditional bariatric surgery — and to weight-loss drugs such as Ozempic and Wegovy — may be on the horizon! Engineers at MIT have designed a new type of gastric balloon that allows individuals to inflate and deflate as needed. In an animal study, the researchers showed that blowing up the balloon before a meal caused rodents to reduce their food intake by 60 percent. Like traditional
gastric balloons, the new design is a silicone balloon filled with air or saline and placed inside the stomach. Both encourage weight loss by giving people a
That’s when the MIT team formulated the idea for the new balloon. It’s inserted into the stomach through an incision in the abdominal wall, then connected to an external controller that’s attached to the skin and contains a pump that inflates and deflates the balloon when needed. The gastric balloon could be an option for patients who are not good candidates for traditional bariatric surgery or don’t respond well to weight-loss drugs, says Traverso.
balloons do work initially,” says

The device is an alternative to Ozempic and other meds feeling of fullness so that they don’t overeat. With old-school gastric balloons, however, their effectiveness eventually wears off as the stomach gets used to the sensation of fullness. “[Traditional] gastric
MIT’s Giovanni Traverso. “Historically, what has been seen is that the balloon is associated with weight loss. But then in general, the weight gain resumes the same trajectory. “What we reasoned was perhaps if we had a system that simulates that fullness in a transient way, meaning right before a meal, that could be a way of inducing weight loss.”


Giovanni Traverso

system function must match at least half of those proteins on the recipient’s cells to be a good fit. Patients are first treated with low doses of chemotherapy and given total body irradiation. Afterward, they take drugs to prevent their immune cells from attacking the donor’s. Of the 42 people with severe sickle cell disease who participated in the study, 95 percent were alive two years after the transplant, and 88 percent were considered cured. “Many people — and maybe most adults — aren’t eligible for gene therapy because of the requirement for high-dose chemotherapy,” says Johns Hopkins Kimmel Cancer Center’s Dr. Richard Jones. But most patients ARE eligible for the transplant, which costs a fraction of the price of gene therapy, he says.
A BREAKTHROUGH bone marrow transplant may finally offer a cure for sickle cell disease, offering hope to the 1 million Americans who suffer from the painful, sometimes life-threatening condition. Researchers at Johns Hopkins University believe this offers a less costly alternative to gene therapy for sickle cell patients — and is more effective than previously available treatments. During the procedure,

The new procedure is less costly than gene therapy

called reducedintensity haploidentical bone marrow transplantation, bone marrow is donated by a “half-matched” relative, such as a parent, sibling, child, aunt or uncle. The proteins that help the donor’s immune
Dr. Richard Jones
NE AMERICA’S MOST TALKED ABOUT MAGAZINE 32 NATIONAL APRIL 7 , 2025